Tooth pain can sometimes be very debilitating, especially if there is an infection associated with it. There are several types of tooth pain, ranging from a dull, pulsating sensation to a sharp, jolt-like agony that makes you jump out of your chair. The causes of tooth pain can vary greatly and can sometimes be difficult to locate and diagnose. Below is a description of the most common problem that causes a tooth ache and how it is diagnosed and treated.
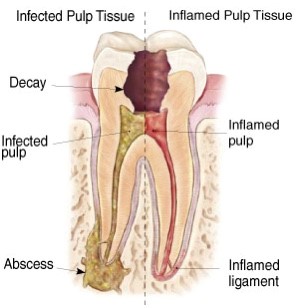
Each tooth is composed of an outer hard enamel layer, an internal softer dentin layer, and a central pulp chamber which houses the pulp of the tooth. In its simplest form, the pulp is made up of a combination of nerve and vascular tissues that help maintain vitality of the tooth. The nerve in the pulp is unique as it can only transmit signals of pain to the brain, which is why very cold things, very hot things, very sweet things, and strong vibrations (aka a dental drill) provoke the same time of feeling... ouch! Although it can be uncomfortable and sometimes intense, it is normal to exhibit this response to the described stimuli. It is when pain lingers minutes or hours after the tooth is provoked by cold, hot, or sweet things, that can be a beginning sign of a bigger problem.
The pulp or nerve of the tooth is most happy when it totally sealed by the enamel and dentin layers of the tooth. When the enamel and dentin layers are breached by a cavity or a crack, the tooth may exhibit slightly stronger sensitivity to cold or hot things which doesn’t linger longer than a few seconds. This can usually be treated with something simple like a filling or a crown depending on the size of the cavity or crack. If the tooth is penetrated all the way through the enamel and dentin layers in to the pulp chamber, the nerve may exhibit a prolonged pain to cold and hot things that lingers with a dull, achy, pulsing sensation minutes to hours afterwards. This means bacteria and its toxins have infected the pulp of the tooth, causing an inflammatory response. Pressure from inflammation and reaction to bacterial toxins cause nerve fibers in the pulp to fire, relaying the signal of bad news to the brain. After prolonged exposure to trauma from bacterial infection, the pulp succumbs and dies. At this point, pain can often stop as there is no longer a vital nerve that can communicate to the brain – often a misconception that the tooth is fine and no longer needs treatment.
It is commonly heard from patients “Doc, my tooth was killing me over the weekend...I couldn’t eat or drink anything. It was driving me crazy I couldn’t sleep – I was up all night! But then I woke up today and it feels totally fine. Cold stuff doesn’t bother it anymore, just a little sore when I chew.” When a tooth ache goes away on its own, it is understandable that further treatment may seem unnecessary. Patients who fall into wishful thinking likely find out sooner or later that the problem is still evident.
As bacteria feast on the dead pulpal tissue inside the tooth, toxins and gasses can build up in the tooth as the bacteria multiply. They then make their way from inside to the tooth, through the canals and out the root(s) of the tooth into the surrounding bone of the jaw. The second phase or wave of the tooth ache usually begins at this point as nerve fibers surrounding the roots of the tooth relay signals of pain. As the body tries to fight off the bacteria and its toxins, a painful dental abscess can form which can lead to facial swelling and swollen glands. It is important that if tooth infection progresses to this stage that treatment is pursued immediately as swelling can become so severe that breathing and swallowing are compromised.
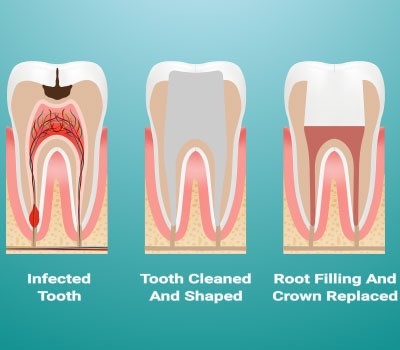
At this stage, the only way to fix the problem is to remove the source of infection, or the diseased nerve inside the tooth. This is done with a procedure called a root canal, where the endodontist drills a hole through the top of the tooth through enamel and dentin, into the pulp chamber of the tooth. With slender instruments called hand files and irrigation with antiseptic solution, the root canals are debrided of diseased nerve tissue and bacteria. The canals are then sealed up with a rubber material which fills the canal space where the nerve used to live, preventing any bacteria from reentering the tooth.
Patients will often ask, “Why do I have to do a root canal, won’t an antibiotic take care of it?” This is a great question, as most infections of the body are treated and cleared with some type of antibiotic treatment. Antibiotics need blood supply to take them to their designated destination to effectively treat infection. They are able to travel through the blood vessels in the jaw surrounding the roots of the infected tooth but will not be able to travel inside the canals of the tooth where the infection began in the first place. A patient will often feel back to normal after taking antibiotics, but once the course is finished and cleared from the body the infection process begins again unless combined with root canal therapy or tooth extraction.
Hopefully this blog helped shed some light on the dreaded tooth ache and why it is important to be seen by your dentist as soon as symptoms develop.
By Dr. Steve DiReda